ઘૂંટણ વિભાગ
હોમ » મુખ્ય વિભાગો » ટોટલ ની જોઈન્ટ રિપ્લેસમેન્ટ (TKR) સર્જરી
સર્જિકલ સારવાર
આર્થ્રોસ્કોપિક સર્જરી: આ ન્યૂનતમ આક્રમક પ્રક્રિયામાં ઘૂંટણની સાંધાની આસપાસ નાના ચીરાઓ દ્વારા નાના કેમેરા (આર્થ્રોસ્કોપ) અને વિશિષ્ટ સર્જિકલ સાધનોનો સમાવેશ થાય છે. આર્થ્રોસ્કોપિક સર્જરીનો ઉપયોગ વિવિધ હેતુઓ માટે થઈ શકે છે, જેમાં નીચેનાનો સમાવેશ થાય છે:
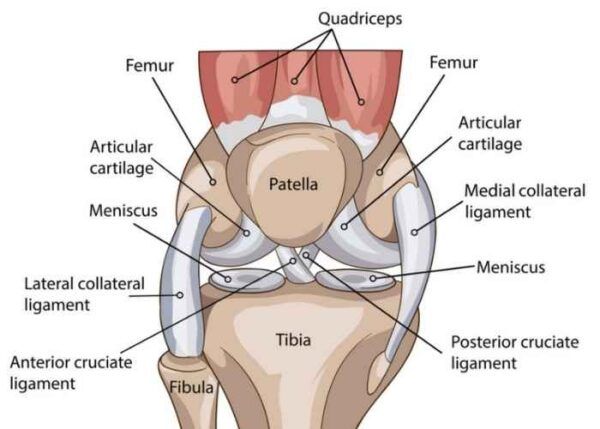
- મેનિસેક્ટોમી: ઘૂંટણમાં મેનિસ્કસ (કોલાસ્થિ) ના ક્ષતિગ્રસ્ત ભાગોને દૂર કરવું.
- મેનિસ્કસ સમારકામ: ફાટેલા મેનિસ્કલ પેશીને સીવ અથવા એન્કરનો ઉપયોગ કરીને સમારકામ.
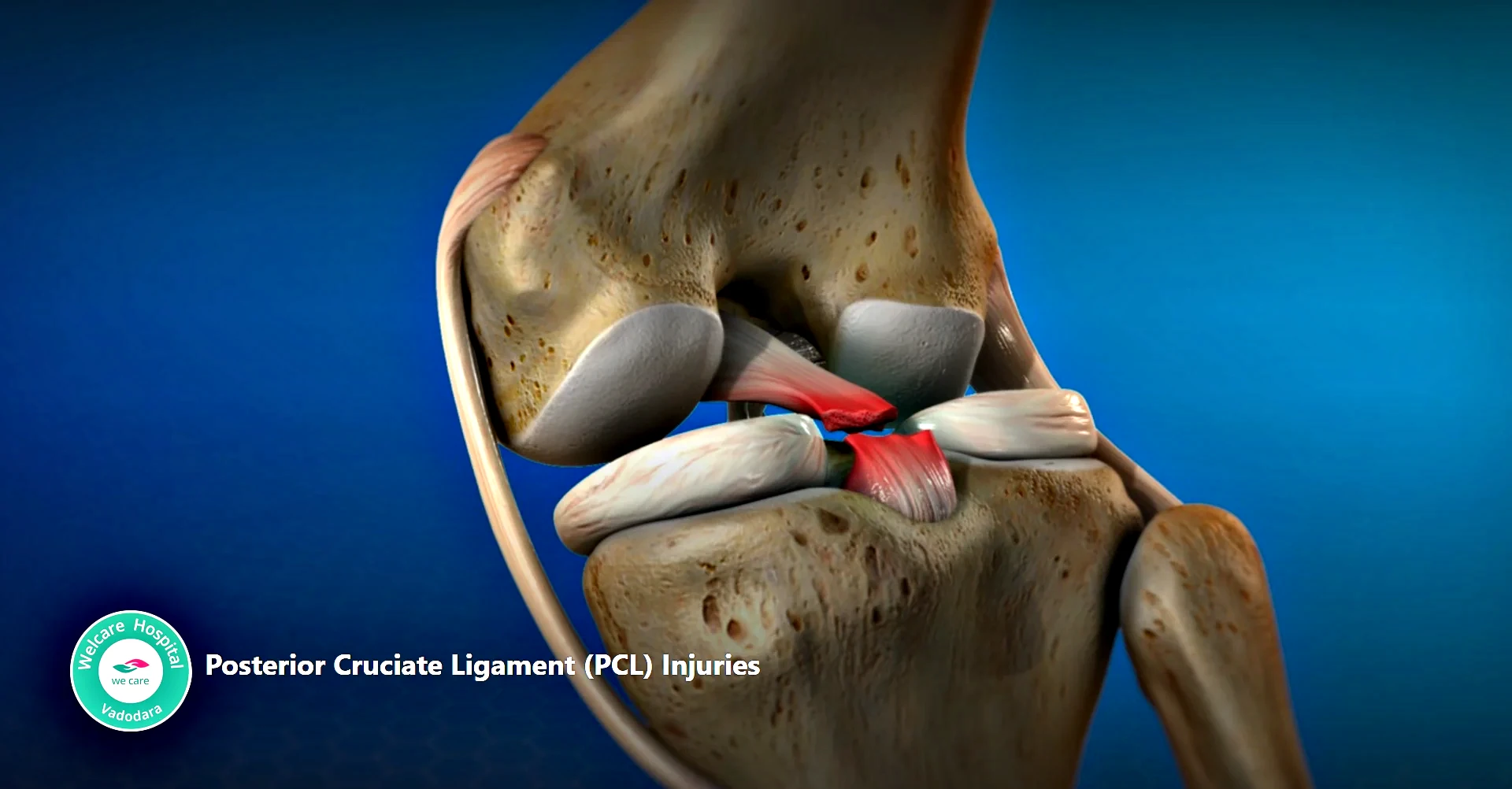
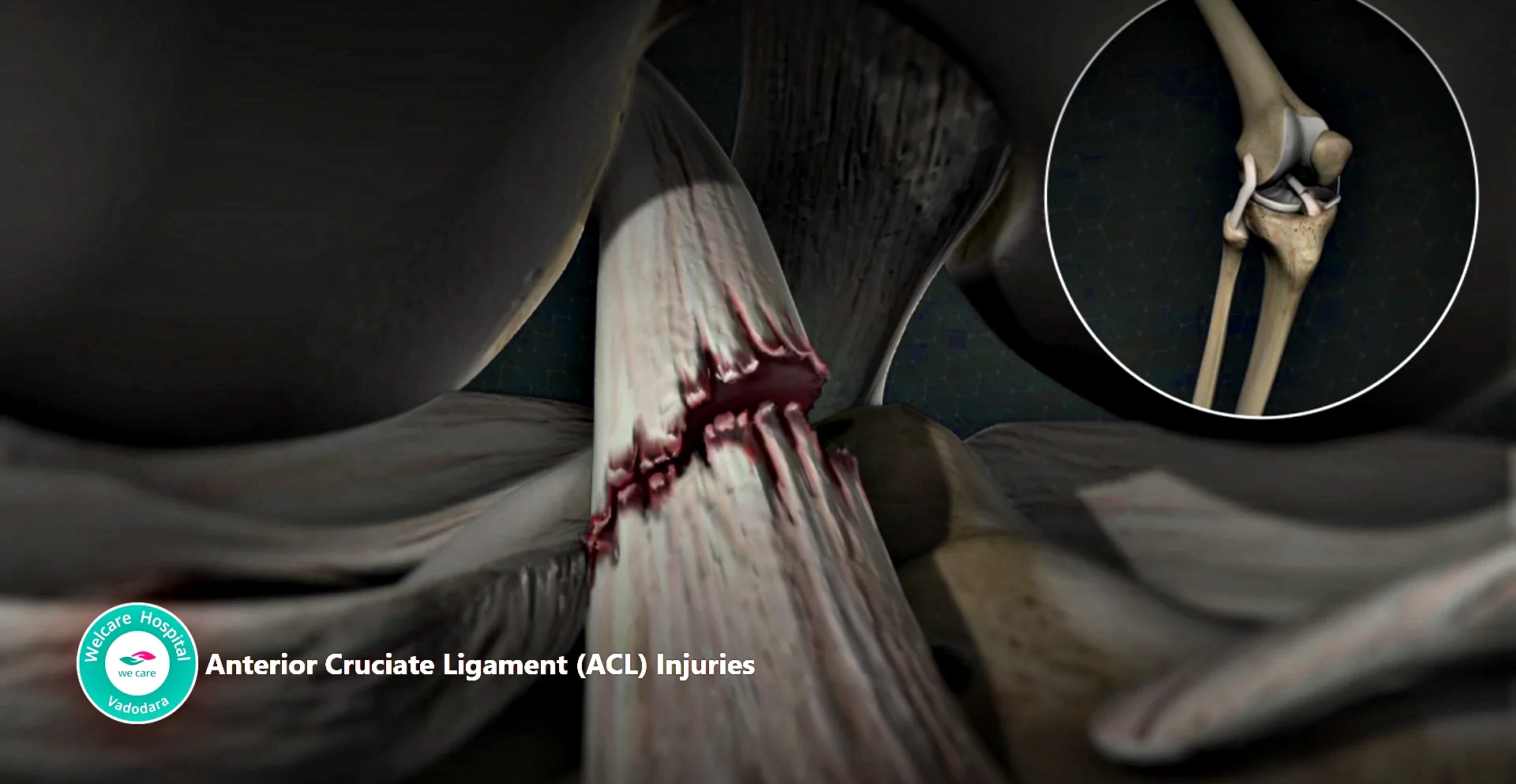
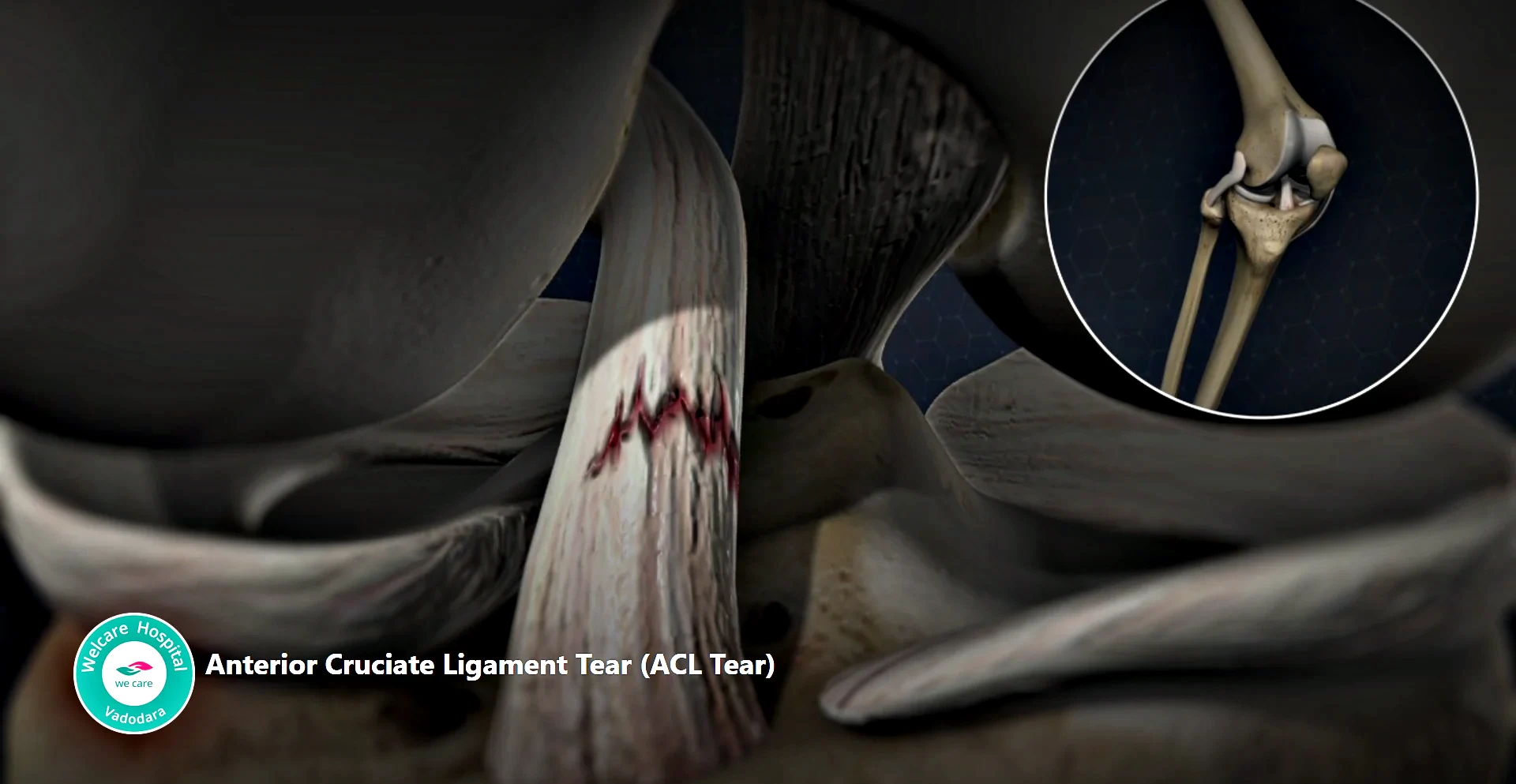
- અસ્થિબંધન પુનઃનિર્માણ: અગ્રવર્તી ક્રુસિએટ લિગામેન્ટ (ACL) અથવા પશ્ચાદવર્તી ક્રુસિએટ લિગામેન્ટ (PCL) જેવા ફાટેલા અસ્થિબંધનનું સમારકામ અથવા પુનઃનિર્માણ.
ઘૂંટણની રિપ્લેસમેન્ટ સર્જરી (આર્થ્રોપ્લાસ્ટી): ગંભીર સંધિવા અથવા સાંધાના નુકસાનના કિસ્સામાં, ઘૂંટણ બદલવાની સર્જરી જરૂરી હોઈ શકે છે. ત્યાં ઘણા પ્રકારો છે:
- ટોટલ ની રિપ્લેસમેન્ટ (TKR): ઘૂંટણના સાંધાની ક્ષતિગ્રસ્ત સપાટીને મેટલ અને પ્લાસ્ટિકના બનેલા કૃત્રિમ ઘટકોથી બદલવામાં આવે છે.
- આંશિક ઘૂંટણની ફેરબદલી: ઘૂંટણના સાંધાના માત્ર ક્ષતિગ્રસ્ત ભાગને ઈમ્પ્લાન્ટ વડે બદલવામાં આવે છે, જે તંદુરસ્ત હાડકા અને પેશીઓને સાચવે છે.
- પુનરાવર્તન ઘૂંટણની ફેરબદલી: એવા કિસ્સાઓમાં કે જ્યાં અગાઉના ઘૂંટણની ફેરબદલી નિષ્ફળ ગઈ હોય અથવા તેને સુધારણાની જરૂર હોય, ઘટકોને બદલવા અથવા સુધારવા માટે પુનરાવર્તન શસ્ત્રક્રિયા કરવામાં આવી શકે છે.
ઑસ્ટિઓટોમી: આ પ્રક્રિયામાં ઘૂંટણની સાંધાની આસપાસના હાડકાંને ફરીથી આકાર આપવા અથવા ક્ષતિગ્રસ્ત અથવા સંધિવાગ્રસ્ત વિસ્તારો પર દબાણ ઘટાડવાનો સમાવેશ થાય છે. પ્રારંભિક તબક્કાના સંધિવા અથવા ઘૂંટણની વિકૃતિના ચોક્કસ પ્રકારો ધરાવતા નાના, સક્રિય દર્દીઓ માટે તેની ભલામણ કરવામાં આવી શકે છે.
કોમલાસ્થિ પુનઃસ્થાપન પ્રક્રિયાઓ: કોમલાસ્થિને નુકસાન અથવા ખામીના કેન્દ્રીય વિસ્તારો ધરાવતા દર્દીઓ માટે, નવી કોમલાસ્થિ વૃદ્ધિને ઉત્તેજીત કરવા અથવા ક્ષતિગ્રસ્ત પેશીઓને બદલવા માટે વિવિધ તકનીકોનો ઉપયોગ કરી શકાય છે. આમાં શામેલ છે:
- માઇક્રોફ્રેક્ચર: નવા કોમલાસ્થિના વિકાસને પ્રોત્સાહન આપવા માટે હાડકામાં નાના ફ્રેક્ચર્સ બનાવવું.
- ઑટોલોગસ કોન્ડ્રોસાઇટ ઇમ્પ્લાન્ટેશન (ACI): દર્દીમાંથી તંદુરસ્ત કોમલાસ્થિ કોષો લણવા, તેમને પ્રયોગશાળામાં ઉગાડવા, અને પછી તેમને ક્ષતિગ્રસ્ત વિસ્તારમાં રોપવા.
- ઓસ્ટિઓકોન્ડ્રલ ઓટોગ્રાફટ અથવા એલોગ્રાફ્ટ ટ્રાન્સપ્લાન્ટેશન: ક્ષતિગ્રસ્ત વિસ્તારને સુધારવા માટે દર્દીના પોતાના શરીરના બીજા ભાગ (ઓટોગ્રાફ) અથવા દાતા (એલોગ્રાફ્ટ) પાસેથી તંદુરસ્ત કોમલાસ્થિ અને હાડકાની પેશીઓનું ટ્રાન્સપ્લાન્ટેશન.
સિનોવેક્ટોમી: ઘૂંટણની સાંધામાં સોજાવાળી સાયનોવિયલ પેશીઓ (સિનોવિયમ) દૂર કરવી, જે ઘણી વખત સંધિવા અથવા અન્ય બળતરા પરિસ્થિતિઓમાં પીડા અને સોજો ઘટાડવા માટે કરવામાં આવે છે.
ઘૂંટણની વિવિધ સમસ્યાઓના નિવારણ માટે ઉપલબ્ધ સર્જિકલ વિકલ્પોના આ માત્ર થોડા ઉદાહરણો છે. શસ્ત્રક્રિયાની પસંદગી અંતર્ગત સ્થિતિ, નુકસાનની માત્રા, દર્દીની ઉંમર અને પ્રવૃત્તિનું સ્તર અને સારવારના લક્ષ્યો જેવા પરિબળો પર આધાર રાખે છે. સૌથી યોગ્ય કાર્યવાહી નક્કી કરવા માટે દર્દીઓએ તેમના ઓર્થોપેડિક સર્જન સાથે તેમના વિકલ્પોની સંપૂર્ણ ચર્ચા કરવી જરૂરી છે.
વેલકેરની ઇન-હાઉસ 3D પ્રિન્ટીંગ લેબ
રોબોટિક આસિસ્ટેડ ની રિપ્લેસમેન્ટના ફાયદા
- હાડકાની કોઈ વધારાની ખોટ માત્ર ક્ષતિગ્રસ્ત ભાગને બદલવામાં આવે છે
- નાનો ચીરો
- સોફ્ટ પેશીને કોઈ નુકસાન થતું નથી
- કોઈ અસ્થિબંધન ઈજા
- પ્રાયોગિક રીતે આજીવન સ્થાયી ઇમ્પ્લાન્ટ
- ઓછી રક્ત નુકશાન
- ઓછી પીડા
- સર્જિકલ સમય માત્ર 10 મિનિટ વધુ
- તે જ દિવસે ચાલવું અને દાદર ચઢવું
- હોસ્પિટલમાંથી વહેલા ડિસ્ચાર્જ
- એમ્બોલિઝમ અથવા DVT ની ઘણી ઓછી તકો
- ઝડપી પુનઃપ્રાપ્તિ
વારંવાર પૂછાતા પ્રશ્નો
શું ઘૂંટણ બદલવા માટે યોગ્ય સમય છે?
ઘૂંટણની બદલી ક્યારે કરવી તે નક્કી કરવા માટે કોઈ ચોક્કસ ફોર્મ્યુલા નથી. તે કરાવવાનું મુખ્ય કારણ પીડા છે. જો તમે જીવનશૈલી વ્યૂહરચનાઓ, બળતરા વિરોધી દવાઓ, શારીરિક ઉપચાર અને ઇન્જેક્શન સહિતના અન્ય વિકલ્પોનો પ્રયાસ કર્યો હોય, તો તે સર્જરી વિશે વિચારવાનો સમય હોઈ શકે છે.
ઓર્થોપેડિક સર્જન સંપૂર્ણ તપાસ કરશે અને ભલામણ કરશે. તમે બીજો અભિપ્રાય પણ મેળવવા માગી શકો છો.
શું હું સર્જરીથી ટાળી શકું?
તમે શસ્ત્રક્રિયા પર વિચાર કરો તે પહેલાં, તમારા ડૉક્ટર સામાન્ય રીતે તમને વિવિધ નોન-સર્જિકલ સારવાર અજમાવવા માટે પ્રોત્સાહિત કરશે, જેમાં શામેલ હોઈ શકે છે:
- શારીરિક ઉપચાર
- વજન ઘટાડવું (જો યોગ્ય હોય તો)
- બળતરા વિરોધી દવા
- સ્ટેરોઇડ ઇન્જેક્શન
- હાયલ્યુરોનિક (જેલ) ઇન્જેક્શન
- વૈકલ્પિક સારવાર જેમ કે એક્યુપંક્ચર
કેટલાક કિસ્સાઓમાં, આ ઉકેલો ઘૂંટણની સમસ્યાઓનું સંચાલન કરવામાં વિશ્વસનીય સ્ત્રોતને મદદ કરી શકે છે. પરંતુ જો લક્ષણો વધુ ખરાબ થાય અને તમારા જીવનની ગુણવત્તાને અસર કરવાનું શરૂ કરે, તો શસ્ત્રક્રિયા શ્રેષ્ઠ વિકલ્પ હોઈ શકે છે. લાંબા સમય સુધી શસ્ત્રક્રિયામાં વિલંબ અથવા ટાળવાથી વસ્તુઓ વધુ ખરાબ થઈ શકે છે.
તમારી જાતને પ્રશ્નો પૂછો જેમ કે:
- શું મેં બધું જ અજમાવ્યું છે?
- શું મારો ઘૂંટણ મને જે વસ્તુઓનો આનંદ માણે છે તે કરવાથી રોકે છે?
- શું ઘૂંટણની ફેરબદલી મારા જીવનની ગુણવત્તામાં સુધારો કરશે?
સર્જરી દરમિયાન શું થાય છે અને તે કેટલો સમય લે છે?
સર્જન તમારા સાંધાના ક્ષતિગ્રસ્ત વિસ્તારને બહાર કાઢવા માટે તમારા ઘૂંટણના આગળના ભાગમાં એક ચીરો બનાવે છે. તેઓ તમારા ઘૂંટણની ટોપીને બાજુ પર ખસેડે છે અને ક્ષતિગ્રસ્ત કોમલાસ્થિ અને થોડી માત્રામાં હાડકાને કાપી નાખે છે.
તે પછી, તેઓ ક્ષતિગ્રસ્ત પેશીઓને નવી ધાતુ અને પ્લાસ્ટિકના ઘટકો સાથે બદલી નાખે છે. ઘટકો એક કૃત્રિમ સંયુક્ત બનાવે છે જે જૈવિક રીતે સુસંગત છે અને તમારા કુદરતી ઘૂંટણની હિલચાલની નકલ કરે છે.
ઘૂંટણ બદલવાની મોટાભાગની પ્રક્રિયાઓને પૂર્ણ થવામાં 1 થી 2 કલાકનો સમય લાગે છે.
કૃત્રિમ ઘૂંટણ એટલે શું?
કૃત્રિમ ઘૂંટણના પ્રત્યારોપણમાં મેટલ અને મેડિકલ-ગ્રેડ પ્લાસ્ટિકનો સમાવેશ થાય છે જેને પોલિઇથિલિન કહેવાય છે.
હાડકામાં ઘટકોને જોડવાની બે રીત છે. એક હાડકાના સિમેન્ટનો ઉપયોગ કરવો, જે સામાન્ય રીતે સેટ થવામાં લગભગ 10 મિનિટ લે છે. બીજો એક સિમેન્ટ-મુક્ત અભિગમ છે, જેમાં એવા ઘટકોનો સમાવેશ થાય છે કે જેમાં છિદ્રાળુ કોટિંગ હોય છે જેથી હાડકાને તેમના પર વધવા દે.
કેટલાક કિસ્સાઓમાં, સર્જન એક જ ઓપરેશન દરમિયાન બંને તકનીકોનો ઉપયોગ કરી શકે છે.
શું મારે એનેસ્થેસિયા વિશે ચિંતા કરવી જોઈએ?
કોઈપણ ઓપરેશન જેમાં એનેસ્થેસિયાનો સમાવેશ થાય છે તેમાં જોખમ હોય છે, પરંતુ ગંભીર ગૂંચવણો ભાગ્યે જ જોવા મળે છે.
જો તમારી પાસે ઘૂંટણની સંપૂર્ણ બદલી છે, તો તમારા વિકલ્પો છે:
- સામાન્ય એનેસ્થેસિયા
- કરોડરજ્જુ અથવા એપિડ્યુરલ એનેસ્થેસિયા
- પ્રાદેશિક ચેતા બ્લોક
એનેસ્થેસિયાની ટીમ તમારા માટે સૌથી યોગ્ય વિકલ્પો નક્કી કરશે, પરંતુ ઘૂંટણ બદલવાની મોટાભાગની પ્રક્રિયાઓમાં ઉપરોક્ત પદ્ધતિઓના સંયોજનનો સમાવેશ થાય છે.
હું કઈ પ્રવૃત્તિઓ કરવા સક્ષમ હોઈશ?
મોટા ભાગના લોકોને ઘૂંટણ બદલવાની સર્જરી પછી લગભગ 3 અઠવાડિયા સુધી સહાયક ઉપકરણ (વોકર, ક્રચ અથવા શેરડી)ની જરૂર પડે છે, જો કે તે વ્યક્તિએ વ્યક્તિએ નોંધપાત્ર રીતે બદલાય છે.
તમે 6-8 અઠવાડિયા પછી સ્થિર બાઇક ચલાવવી, ચાલવું અને સ્વિમિંગ જેવી ઓછી અસરવાળી કસરત કરી શકશો. સ્વિમિંગ કરતા પહેલા તમારો ચીરો સંપૂર્ણપણે સાજો થઈ ગયો છે તેની ખાતરી કરવી મહત્વપૂર્ણ છે.
તમારા ભૌતિક ચિકિત્સક તમને આ સમય દરમિયાન નવી પ્રવૃત્તિઓ શરૂ કરવા માટે સલાહ આપી શકે છે. તમારે શસ્ત્રક્રિયા પછી દોડવું, કૂદવાનું અને અન્ય ઉચ્ચ અસરવાળી પ્રવૃત્તિઓ ટાળવી જોઈએ.
મારા કૃત્રિમ ઘૂંટણ ક્યાં સુધી ચાલશે?
2019ની સંશોધન સમીક્ષા મુજબ, કુલ ઘૂંટણની ફેરબદલીના 82% થી વધુ વિશ્વસનીય સ્ત્રોત 25 વર્ષ પછી પણ કાર્ય કરી રહ્યાં છે. પરંતુ ઘસારો અને આંસુ કૃત્રિમ ઘૂંટણની કામગીરી અને આયુષ્ય પર નકારાત્મક અસર કરી શકે છે.
યુવાન લોકોને તેમના જીવનકાળમાં અમુક સમયે ઘૂંટણની બીજી સર્જરીની જરૂર પડવાની શક્યતા વધુ હોય છે, મુખ્યત્વે વધુ સક્રિય જીવનશૈલીના પરિણામે. તમે તમારી ચોક્કસ પરિસ્થિતિ વિશે ડૉક્ટરની સલાહ લઈ શકો છો.
પુનઃપ્રાપ્તિ દરમિયાન હું શું અપેક્ષા રાખી શકું?
મોટાભાગના લોકો વોકર અથવા ક્રેચની મદદથી 24 કલાકની અંદર ઉભા થઈને ચાલતા હોય છે.
તમારા ઓપરેશન પછી, ભૌતિક ચિકિત્સક તમને તમારા ઘૂંટણને વાળવામાં અને સીધો કરવામાં, પથારીમાંથી બહાર નીકળવામાં અને આખરે તમારા નવા ઘૂંટણ સાથે ચાલવાનું શીખવામાં મદદ કરશે. આ ઘણીવાર તમારા ઓપરેશનના દિવસે જ થાય છે.
મોટાભાગના લોકોને શસ્ત્રક્રિયા પછી તે જ દિવસે અથવા સવારે હોસ્પિટલમાંથી રજા આપવામાં આવે છે.
એકવાર તમે ઘરે પાછા ફર્યા પછી, તમે કેટલાક અઠવાડિયા સુધી નિયમિતપણે ઉપચાર કરવાનું ચાલુ રાખશો. તમે વિશિષ્ટ કસરતો કરશો જેનો હેતુ ઘૂંટણની કાર્યક્ષમતામાં સુધારો કરવાનો છે.
જો તમારી સ્થિતિને તેની જરૂર હોય, અથવા જો તમારી પાસે તમને ઘરે જરૂરી સમર્થન ન હોય, તો તમારા ડૉક્ટર ભલામણ કરી શકે છે કે તમે પહેલા પુનર્વસન અથવા નર્સિંગ સુવિધામાં સમય પસાર કરો.
મોટાભાગના લોકો 3 મહિનાની અંદર સ્વસ્થ થઈ જાય છે, જોકે કેટલાક લોકોને સંપૂર્ણ સ્વસ્થ થવામાં 6 મહિના કે તેથી વધુ સમય લાગી શકે છે.