Foot & Ankle
Home » Core Departments » Foot & Ankle
Introduction
The human ankle is a complex joint involving a combination of bones from both the leg and the foot. The ankle itself primarily consists of three bones, but its functionality also involves several other bones in the foot. Here is a detailed list of the bones associated with the ankle and their respective movements.
Understanding these bones and their interconnections is essential for diagnosing ankle injuries, planning surgeries and ensuring effective treatment and rehabilitation of ankle conditions.
Bones in the Human Ankle:
- Tibia (Shinbone): The tibia, or shinbone, is the larger and stronger of the two bones in the lower leg. It bears most of the body’s weight and forms the medial (inner) part of the ankle joint by articulating with the talus.
- Fibula: The fibula is the thinner and smaller bone of the lower leg. It runs parallel to the tibia and forms the lateral (outer) part of the ankle joint by articulating with the talus.
- Talus: The talus is the bone at the top of the ankle that connects the leg to the foot. It articulates with the tibia and fibula, forming the ankle joint, and plays a crucial role in the movement and stability of the ankle.
- Posterior Malleolus: Part of the tibia, the posterior malleolus forms the back part of the ankle joint. It contributes to the stability of the joint and serves as an attachment for ligaments.
Bones in the Foot Connected to the Ankle:
- Calcaneus (Heel Bone Also known as the heel bone, the calcaneus is the largest bone in the foot. It forms the foundation of the rear part of the foot and connects with the talus at the subtalar joint, which allows for inversion and eversion movements of the foot.
- Navicular Bone: Located in front of the talus, the navicular bone is one of the tarsal bones that helps form the arch of the foot and aids in the distribution of weight across the foot.
- Cuboid Bone: : The cuboid bone is another tarsal bone, located on the lateral side of the foot, in front of the calcaneus. It helps stabilize the lateral column of the foot and contributes to the foot’s overall structure.
- Three Cuneiform Bones (Medial, Intermediate, Lateral): There are three cuneiform bones (medial, intermediate, and lateral) located in front of the navicular bone. They help form the transverse arch of the foot and provide stability and flexibility.
- Medial Malleolus: This is the prominence on the inner side of the ankle, formed by the lower end of the tibia. It provides stability to the ankle joint and serves as an attachment point for ligaments.
- Lateral Malleolus: Formed by the lower end of the fibula, the lateral malleolus is the bony bump on the outer side of the ankle. It also provides stability and is a key attachment point for ligaments.
- Navicular Bone: Located in front of the talus, the navicular bone is one of the tarsal bones that helps form the arch of the foot and aids in the distribution of weight across the foot.
- Sesamoid Bones: These are small bones embedded within the tendons of the big toe, not directly part of the ankle but crucial for the function and mechanics of the foot. They help absorb the weight-bearing stress during walking and running.
- Anterior Inferior Tibiofibular Ligament: While not a bone, this ligament connects the tibia and fibula at the ankle, contributing to the stability of the syndesmosis, which is the joint where the two bones meet.
Movements Controlled by the Ankle Joint
- Plantarflexion: This movement involves pointing the toes downward, away from the leg. It is primarily controlled by the interaction between the tibia, fibula, and talus. Muscles such as the gastrocnemius and soleus are involved in this action.
- Dorsiflexion: This is the movement of bringing the toes upward towards the shin. The tibia and fibula articulate with the talus to allow this motion. The tibialis anterior muscle plays a key role in dorsiflexion.
- Inversion: This movement involves turning the sole of the foot inward, towards the midline of the body. It is facilitated by the subtalar joint, which includes the talus and calcaneus. Muscles such as the tibialis posterior and tibialis anterior contribute to inversion.
- Eversion: This is the opposite of inversion, where the sole of the foot is turned outward, away from the midline of the body. The subtalar joint also enables this movement, with the fibularis (peroneus) longus and fibularis (peroneus) brevis muscles playing significant roles.
- Abduction: Movement of the foot away from the midline of the body. This motion is limited in the ankle joint itself but can occur at the subtalar joint and other foot joints.
- Adduction: Movement of the foot towards the midline of the body, similar to abduction but in the opposite direction. Like abduction, it is more prominent in the subtalar and midfoot joints rather than the ankle joint itself.
The coordination of these movements allows for the complex and varied motions required for walking, running, jumping, and maintaining balance. Understanding these bones and their associated movements is essential for diagnosing and treating ankle and foot disorders.
Conditions / Issues
- Achilles tendon: injury, often resulting from overuse or sudden increases in physical activity, is characterized by pain, swelling, and stiffness in the back of the lower leg above the heel. This condition is prevalent among athletes, particularly those engaged in running and jumping sports, and can significantly impair mobility if not properly treated.
- A calcaneus fracture: often caused by high-impact trauma such as falls from a height or motor vehicle accidents, involves a break in the heel bone. This injury can lead to significant pain, swelling, and difficulty bearing weight, often requiring surgical intervention for proper healing and restoration of function.
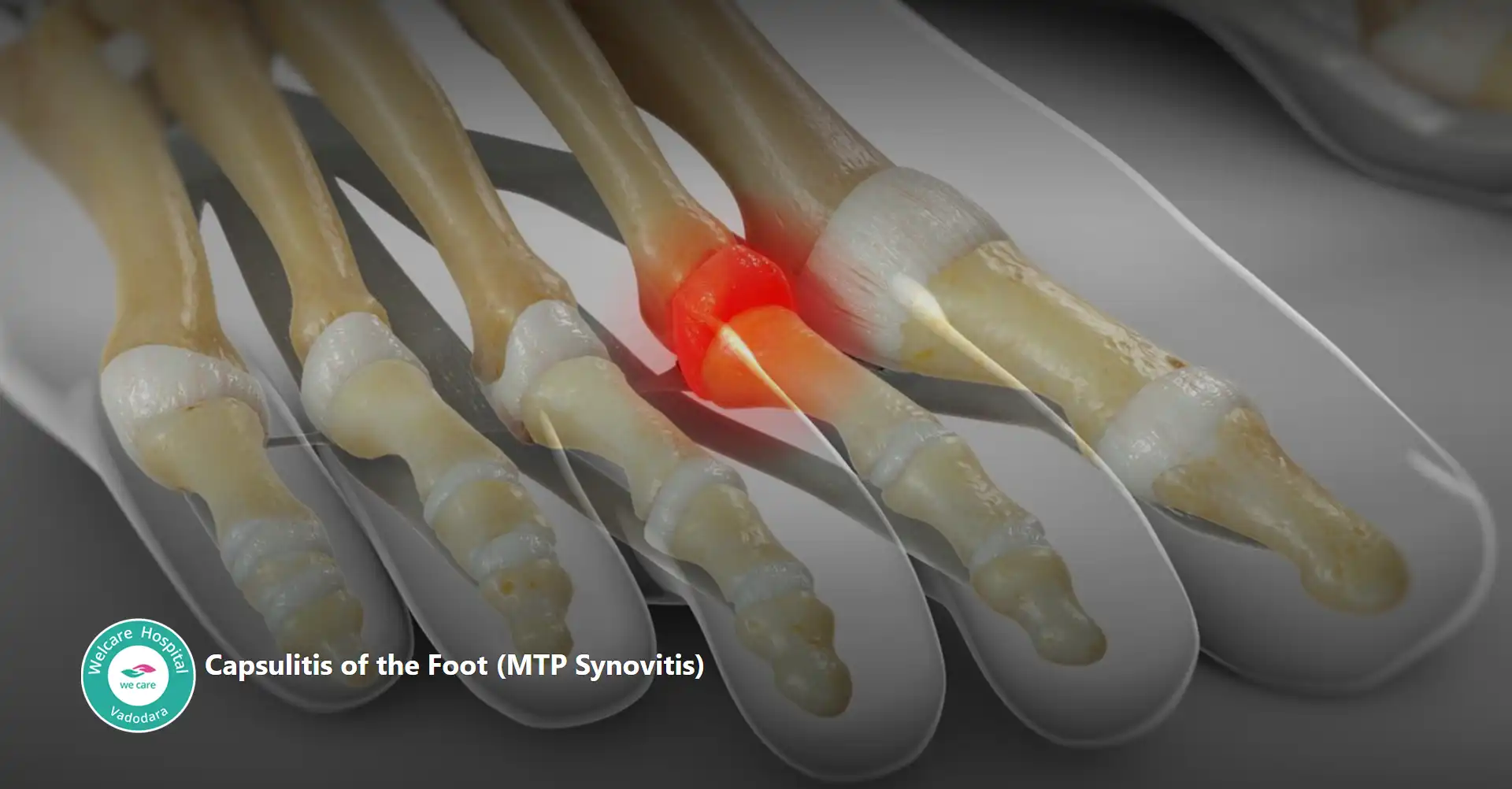
- Capsulitis of the foot: is an inflammatory condition affecting the ligaments around the joint capsule, commonly occurring in the second toe but can affect any toe joint. This condition results in pain, swelling, and difficulty walking, often caused by repetitive stress, improper footwear, or abnormal foot mechanics.
- Club foot: or congenital talipes equinovarus, is a deformity present at birth where one or both feet are twisted out of shape or position. This condition results in the foot being turned inward and downward, resembling the shape of a golf club, which is where the name “club foot” comes from. This deformity affects the bones, muscles, tendons, and blood vessels of the foot, causing significant tightness and rigidity. If left untreated, it can lead to severe mobility issues and pain as the child grows. Early intervention is crucial, typically starting with non-surgical methods such as the Ponseti method, which involves gentle manipulation and casting to gradually correct the position of the foot. In some cases, minor surgical procedures may be necessary to release tight tendons or realign bones. With proper treatment, most children with club foot can achieve good mobility and function.
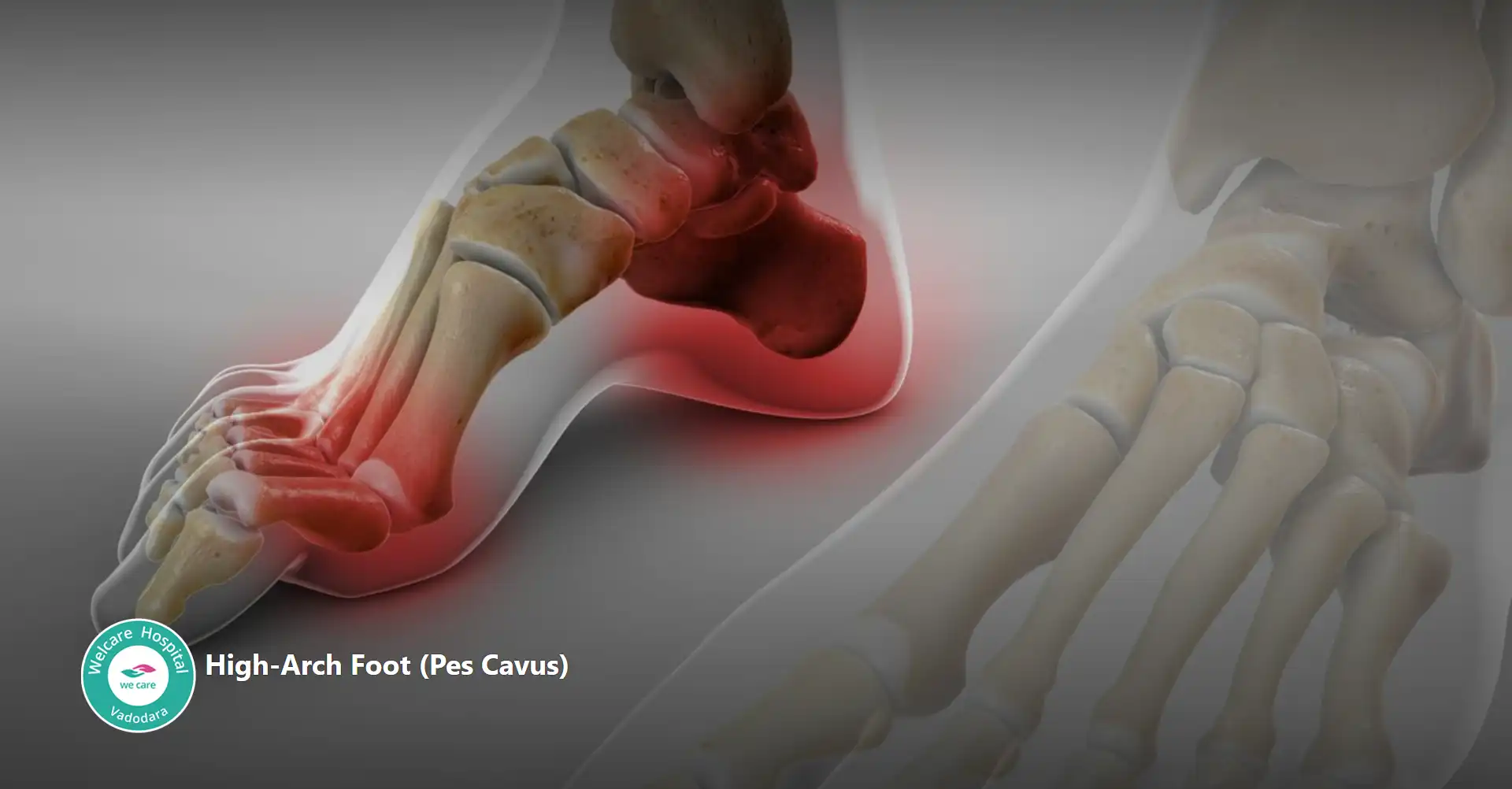
- Pes cavus: also known as high arch foot, is a condition characterized by an unusually high arch in the foot, leading to an excessive amount of weight being placed on the ball and heel of the foot when walking or standing. This condition can be congenital or acquired and is often associated with neurological disorders such as Charcot-Marie-Tooth disease, cerebral palsy, or spina bifida. Individuals with pes cavus may experience foot pain, instability, and an increased risk of ankle sprains. Other common symptoms include calluses on the ball or heel of the foot, hammertoes, and claw toes. Treatment options depend on the severity and underlying cause but may include orthotic devices, physical therapy, and in severe cases, surgical intervention to correct the deformity and improve foot function.
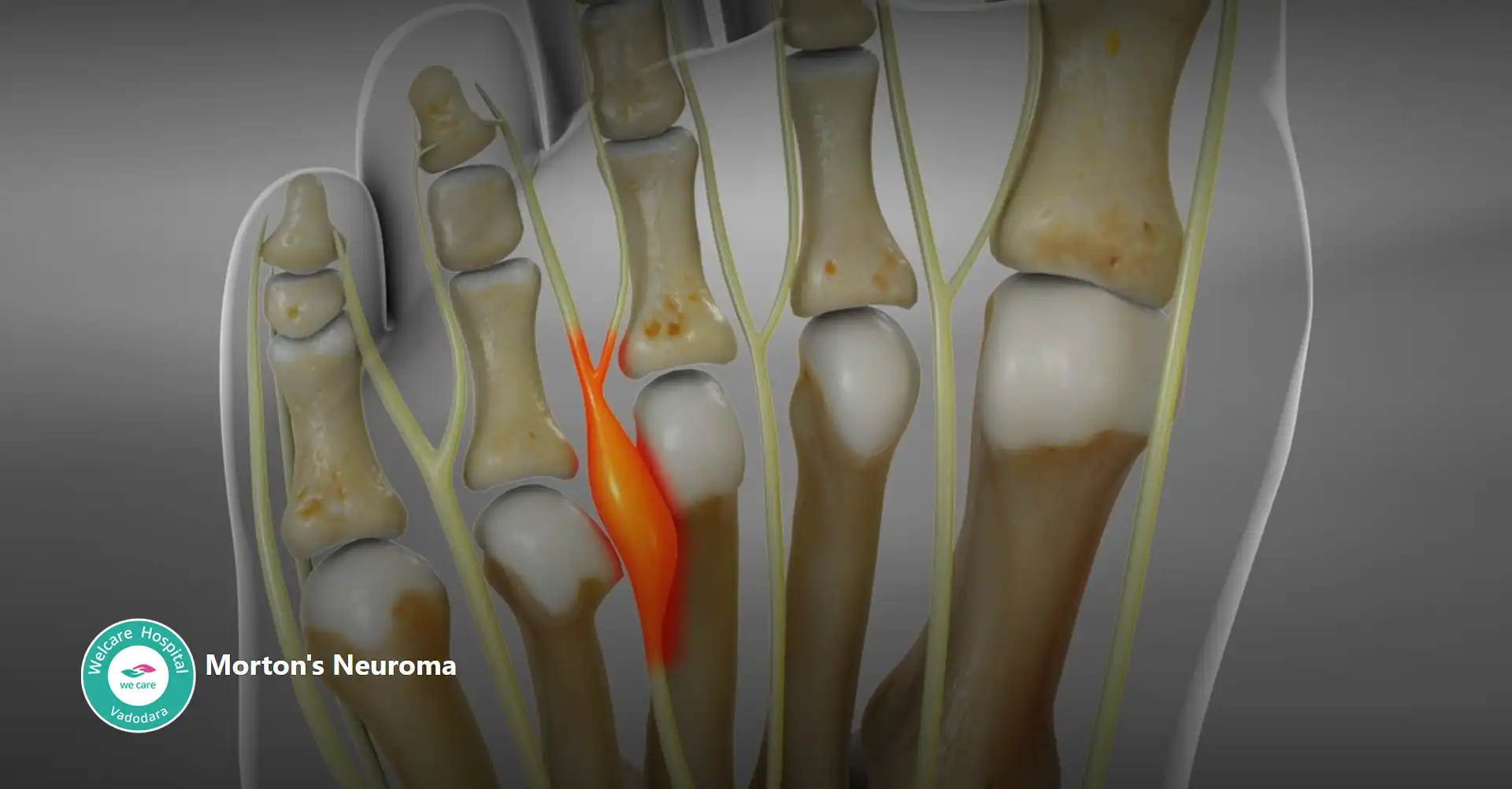
- Morton’s neuroma: is a painful condition that affects the ball of the foot, most commonly between the third and fourth toes. It involves the thickening of the tissue around one of the nerves leading to the toes, which can cause sharp, burning pain, numbness, or a tingling sensation in the affected area. This condition is often associated with wearing tight or high-heeled shoes, which can compress the toes and exacerbate symptoms. Treatment typically includes wearing wider shoes, using orthotic inserts to reduce pressure on the nerve, and, in some cases, corticosteroid injections to reduce inflammation. In severe cases where conservative treatments fail, surgical removal of the affected nerve may be necessary.
- Navicular stress fracture: is a hairline fracture of the navicular bone, located on the top of the midfoot. This type of fracture is commonly seen in athletes who participate in high-impact sports such as running, basketball, and gymnastics due to repetitive stress and overuse. Symptoms of a navicular stress fracture include a vague, aching pain in the midfoot that worsens with activity and improves with rest, as well as tenderness over the navicular bone. Diagnosis often requires imaging studies such as MRI or bone scan, as plain X-rays may not always reveal the fracture. Treatment typically involves a period of rest and immobilization, often using a cast or boot to allow the bone to heal, followed by a gradual return to activity under the guidance of a healthcare professional. In some cases, surgical intervention may be necessary if conservative treatment fails to achieve proper healing.
- Osteochondral lesion of the talus: also known as osteochondritis dissecans (OCD) of the talus, is a condition involving damage to the cartilage and underlying bone of the talus bone in the ankle joint. This can occur due to a traumatic injury, repetitive microtrauma, or inadequate blood supply to the affected area.
Symptoms of an osteochondral lesion of the talus include pain, swelling, and stiffness in the ankle joint, as well as a catching or locking sensation during movement. If left untreated, it can lead to further damage to the cartilage and bone, resulting in chronic pain and limited mobility. - Peroneal tendinosis: is a condition characterized by degeneration, inflammation, or damage to the peroneal tendons, which can result from overuse, trauma, or biomechanical issues. Peroneal tendons located on the outside of the ankle. Symptoms of peroneal tendinosis include pain, swelling, and tenderness along the outside of the ankle, especially during activities such as walking, running, or standing on tiptoes. If left untreated, it can lead to weakness, instability, and an increased risk of ankle sprains.
- Pilon fracture: is a severe type of ankle fracture that involves the lower end of the tibia (shinbone) where it meets the talus (ankle bone). These fractures typically occur as a result of high-energy trauma, such as a fall from height or a motor vehicle accident. Pilon fractures often result in significant displacement of the ankle joint and can be associated with extensive soft tissue damage. Symptoms include severe pain, swelling, deformity, and difficulty bearing weight on the affected limb.
- Plantar fasciitis: is a common condition characterized by inflammation of the plantar fascia, a thick band of tissue that runs along the bottom of the foot, connecting the heel bone to the toes. It is one of the most frequent causes of heel pain, especially with the first steps in the morning or after long periods of rest. The primary symptom of plantar fasciitis is sharp pain in the heel or along the arch of the foot, which can be exacerbated by activities that put stress on the plantar fascia, such as standing, walking, or running. Risk factors for developing plantar fasciitis include overuse, flat feet, high arches, obesity, tight calf muscles, and wearing shoes with inadequate support.
- Sesamoiditis: is a painful condition characterized by inflammation of the sesamoid bones, which are small, pea-shaped bones located beneath the big toe joint within the tendons. These bones help to bear weight and provide leverage for the tendons, particularly during activities like walking, running, and jumping. The primary symptom of sesamoiditis is pain in the ball of the foot, typically beneath the big toe joint. The pain may be dull or sharp and can worsen with activities that involve pushing off the toes, such as walking, running, or bending the big toe. Sesamoiditis often occurs due to repetitive stress or overuse, such as participating in high-impact sports or activities that involve excessive pressure on the forefoot. Other contributing factors may include wearing high-heeled shoes, having a high arch or rigid foot structure, or engaging in activities that require repetitive bending of the big toe.
- Talus fracture: is a break in the talus bone, which is located at the top of the foot, between the heel bone (calcaneus) and the tibia and fibula bones of the lower leg. Talus fractures are relatively uncommon but can occur due to high-energy trauma such as car accidents, falls from height, or sports injuries. Symptoms of a talus fracture include severe pain, swelling, and difficulty bearing weight on the affected foot. Depending on the severity and location of the fracture, there may also be visible deformity or instability of the ankle joint.
- Tibial fracture: is a break in the tibia bone, also known as the shinbone, which is one of the two long bones in the lower leg. Tibial fractures can occur at any point along the length of the tibia, from the knee to the ankle, and can vary in severity from simple cracks in the bone to complete breaks with displacement of the bone fragments. Symptoms of a tibial fracture include severe pain, swelling, bruising, and deformity of the lower leg. Depending on the location and type of fracture, there may also be difficulty bearing weight on the affected leg and an inability to move the foot or toes.
Surgical Treatments
Depending upon the condition and severity of the issue Welcare Hospital at Vadodara has facility for various Surgical Treatments for Foot & Ankle.
The following is a broad list:
- Ankle Arthroscopy
- Ankle Ligament Reconstruction
- Ankle Joint Replacement
- Ankle Osteoarthirits
- Malunion Ankle Reconstruction
- Mourtans Neuroma Surgery
- Halux vallgus Surgery
- Flat Valgus Surgery
- Haglund’s Syndrome Surgery
Non Surgical Treatment
Non-surgical treatments for foot conditions are often the first line of defense and can effectively manage many common foot problems. Here are some non-surgical treatments for various foot conditions:
- Rest and Activity Modification: Resting the affected foot and modifying activities that exacerbate symptoms can help reduce pain and inflammation in many foot conditions, such as plantar fasciitis, Achilles tendinitis, and stress fractures.
- Orthotic Devices: Custom orthotic inserts or over-the-counter arch supports can provide support, cushioning, and realignment of the foot to alleviate pain and correct biomechanical issues associated with conditions like flat feet, high arches, and overpronation.
- Footwear Modifications: Wearing supportive and properly fitting footwear with adequate arch support, cushioning, and room for the toes can help relieve pressure and reduce symptoms associated with various foot conditions, including bunions, hammertoes, and neuromas.
- Physical Therapy: Targeted exercises, stretching, and strengthening techniques prescribed by a physical therapist can help improve flexibility, strength, and stability in the foot and ankle, which can aid in the management of conditions such as plantar fasciitis, Achilles tendinitis, and ankle instability.
- Ice Therapy: Applying ice packs or cold therapy to the affected area can help reduce pain, inflammation, and swelling associated with acute injuries, overuse conditions, and inflammatory conditions like plantar fasciitis and arthritis.
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Over-the-counter medications such as ibuprofen (Advil, Motrin) or naproxen (Aleve) can help alleviate pain and reduce inflammation associated with various foot conditions, including arthritis, tendonitis, and bursitis.
- Physical Modalities: Modalities such as ultrasound therapy, electrical stimulation (e.g., TENS), and laser therapy may be used by healthcare professionals to help reduce pain, promote healing, and improve tissue function in the foot.
- Corticosteroid Injections: In some cases, corticosteroid injections may be recommended to reduce pain and inflammation in conditions such as plantar fasciitis, bursitis, and arthritis. However, these injections are typically reserved for short-term relief and may carry risks of side effects with long-term use.
- Shockwave Therapy: Extracorporeal shockwave therapy (ESWT) is a non-invasive treatment option that uses shockwaves to stimulate healing and reduce pain in conditions such as plantar fasciitis and Achilles tendinitis.
- Lifestyle Modifications: Making lifestyle changes such as losing weight, quitting smoking, and improving overall fitness can help reduce stress on the feet and lower the risk of developing or worsening foot conditions such as plantar fasciitis, osteoarthritis, and peripheral neuropathy.
These non-surgical treatments can be highly effective in managing many foot conditions and may be used alone or in combination with other therapies to achieve optimal outcomes. It’s essential to consult with a healthcare professional for a proper diagnosis and personalized treatment plan tailored to your specific needs and goals.